DAP Health’s mission is to provide comprehensive health care and support services where all people are seen, heard, and affirmed — including those who use drugs.
Words by Jacob Anderson-Minshall
In the first seven months of this year, DAP Health has saved the lives of a thousand people. Upon finding someone in crisis, neighbors, friends, loved ones, and passersby have used nasal naloxone (brand name Narcan) obtained from the health care nonprofit to reverse overdoses.
That is harm reduction. And it works. Using evidence-based strategies can minimize the negative consequences of drug use.
To understand why harm reduction is an essential element of DAP Health’s services, we have to travel back to the 1980s — during the dark days of the AIDS crisis, when once healthy, young Americans were reduced to shades of themselves before passing away. The disease’s quick progression drove fear and paranoia, but there were also those all but cheering the disease on as it ravaged disadvantaged communities of gay men, sex workers, and drug users. Doctors refused to treat us, funeral directors refused to bury us. Our countrymen seemed happy to see us die.
It was in this toxic environment that Desert AIDS Project (now DAP Health) was founded to serve the most reviled people in the nation — those with AIDS-related conditions. In the public eye, those patients were the lowest of the low. But to DAP, “they” were us. And our loved ones. Precious human beings who deserved to be treated with care and respect, regardless of what they had or hadn’t done.
“Essentially, we are doing the same work of early response to AIDS,” muses DAP Health Harm Reduction Supervisor Neil Gussardo. “We care for people who are, at best, misunderstood by the larger community.”
DAP Health’s harm reduction philosophy is integrated, because reducing harm is an essential part of health care. It’s a compassionate approach that improves broader well-being without pretending drug use and addiction aren’t widespread. It’s also tailored without demanding abstinence.
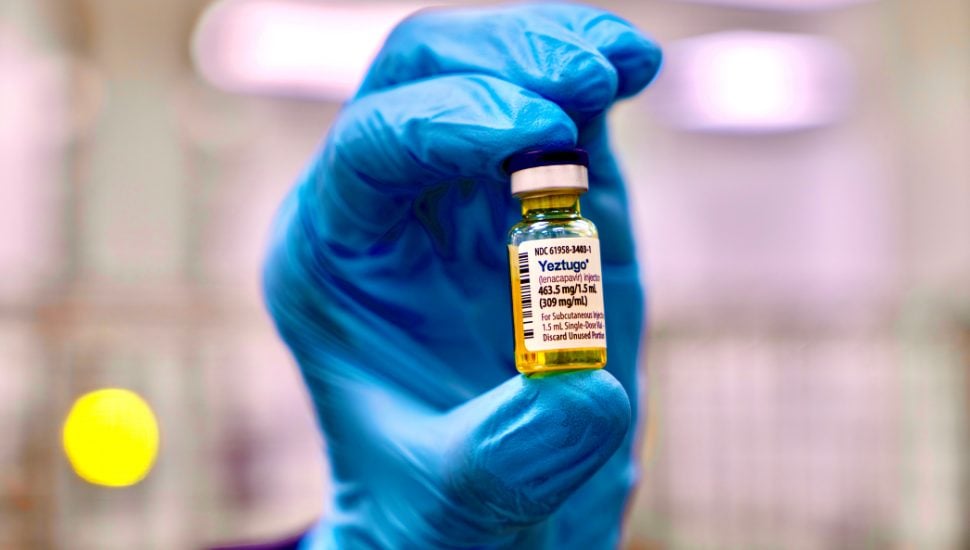
“We engage participants with respect and dignity,” continues Gussardo, “and strive to save lives and improve community health and safety by providing naloxone, fentanyl test strips, and access to sterile use equipment. We increase connections to care, including medical, mental health, and substance use disorder treatment.”
Five Myths About Harm Reduction
According to Gussardo, they are:
1 – Harm reduction encourages drug use
Reality: Harm reduction doesn’t promote or encourage drug use — it accepts that drug use exists and focuses on reducing the negative consequences (e.g., overdose, disease transmission). It’s about safety, not approval.
2 – It’s only about drug use
Reality: While it’s often associated with substance use (like needle exchange or safe consumption sites), harm reduction applies broadly: sex work, mental health, self-injury, even driving safety (e.g., seatbelts). It’s a public health philosophy, not a niche practice.
3 – It’s a ‘soft’ or ‘enabling’ approach
Reality: It’s actually pragmatic and evidence-based. Harm reduction meets people where they are, recognizing that not everyone is ready or able to stop risky behaviors. It prioritizes survival, dignity, and autonomy — often achieving better long-term outcomes than abstinence-only approaches.
4 – People who use harm reduction services aren’t trying to get better
Reality: Many are — just on their own terms. Harm reduction can be a pathway to recovery, but doesn’t make recovery a condition for help. It respects personal goals, whether that’s abstinence, reduced use, or just staying alive.
5 – It doesn’t work
Reality: Numerous studies show it does work:
- Syringe service programs reduce HIV and hepatitis C.
- Naloxone access saves lives from opioid overdoses.
- Harm Reduction connects people to care.
How to Administer Narcan
You too can save a life.
While fentanyl remains of utmost concern, and most likely to be the cause of an overdose, the introduction of a new drug xylazine (a veterinary anesthetic and sedative that’s not intended for human use) has complicated things. First, it is not an opiate, therefore naloxone will not reverse an overdose. That said, Gussardo maintains he still encourages the use of naloxone because fentanyl and xylazine are frequently mixed together and the naloxone will still reverse the effects of fentanyl.
Intervening on an overdose can be as easy as these seven steps:
1 – Approach the person asking, “Are you OK? Can you hear me?”
2 – Look for signs of breathing. If breathing is super shallow (or absent), and the person is unresponsive, move to step 3.
3 – Say, “Hey, my friend, I’m going to Narcan you!” (Use the brand name because it has the widest recognition.)
4 – Use one application of nasal naloxone (generic, or brand name Narcan).
5 – Call 911, because naloxone typically wears off in 30-90 minutes, and opioids can remain in the body for much longer. Emergency medical professionals can monitor the individual and continue care.
6 – Provide rescue breathing, if needed.
7 – After two minutes, if the person still isn’t breathing, give a second dose.
To learn more about DAP Health’s harm reduction services, please click here.