This August, National Immunization Awareness Month reminds us: vaccines keep you, your loved ones, and our community healthy.
Words by Maggie Downs
When Dr. Bernard Wosk of DAP Health talks about vaccines, he doesn’t speak in abstractions. He speaks from experience. “I come from a third world country, and I saw the devastation of infectious diseases in a way that most people in the United States are not exposed to,” says the pediatrician who practices at DAP Health’s Centro Medico Escondido. “I still get chills when I think about seeing the neighbor who died of tetanus. I was 6 years old. My other neighbor died of polio.”
While Wosk was growing up in Nicaragua, these tragedies weren’t rare. They were part of life in a community without widespread vaccination. And Wosk knows the United States once looked much the same. In the early 20th century, before routine childhood immunization, preventable diseases claimed the lives of thousands of American children each year.
That’s why the recent resurgence of certain illnesses feels to him both personal and preventable. It’s a public health setback that echoes a past the country worked hard to leave behind. “Fortunately, the vast majority of my patients do believe in vaccines,” he says. “I consider myself the vaccine doctor, because I convince people who are not vaccinated to get vaccinated. It’s too important.”
The rise of skepticism
The slide in vaccine confidence began during the COVID-19 pandemic, when political divides, misinformation, and high-profile skeptics, including Health and Human Services Secretary Robert F. Kennedy Jr., eroded public trust. The Centers for Disease Control and Prevention reports that vaccination coverage for children born in 2020 and 2021 was lower than for those born in 2018 and 2019, with most vaccines seeing declines of 1.3 to 3.2 percentage points.
That may sound like a small dip. But for highly contagious diseases like measles, even a 1% change can weaken herd immunity. Recent U.S. measles outbreaks have been traced to unvaccinated individuals, in some cases leading to avoidable deaths.
“Maybe being unvaccinated doesn’t affect the child. But that action could affect someone who is more vulnerable, who then gets sick, who’s then hospitalized, who then passes away,” says Nikki Washington, the immunization coordinator for DAP Health. “You end up with a more serious — or deadly — situation that could have been prevented.”
The measles, mumps, and rubella (MMR) vaccine offers about 97% protection and has decades of safety data behind it. Every child who gets it helps shield not only themselves, but also classmates, neighbors, and those whose health prevents them from being vaccinated.
History also offers a powerful counterpoint to any hesitancy. Smallpox, a disease that once killed millions, was eradicated by coordinated vaccination efforts. Polio, which paralyzed thousands of American children each year, is so rare now that most young doctors have never seen a case.
Adults need vaccines too
Vaccine schedules are set by the Advisory Committee on Immunization Practices (ACIP), a panel of about 15 pediatricians, immunologists, scientists, and other vetted experts who serve voluntarily and review decades of safety and effectiveness data. Their recommendations cover every stage of life, from a baby’s first months to older adulthood.
“Every recommended vaccine is there for a reason,” says DAP Health Director of Infectious Diseases Dr. Shubha Kerkar. “So every one of them is extremely critical.”
Even a complete childhood series doesn’t guarantee lifelong immunity; some vaccines require boosters, while others are first advised later in life. The annual flu shot, for example, reduces the spread of a virus that kills tens of thousands of Americans each year. Adults also need a one-time tetanus, diphtheria, and pertussis (Tdap) shot, followed by a Td or Tdap booster every 10 years. For those over age 50, the shingles vaccine can prevent a painful reactivation of the chickenpox virus, while pneumococcal shots protect against pneumonia and meningitis, both of which can be for older adults or people with chronic illnesses.
“If you’re not sure what you need, a simple blood test, called a titer, can check your immunity for certain vaccines and tell you if you need a booster,” Washington says.
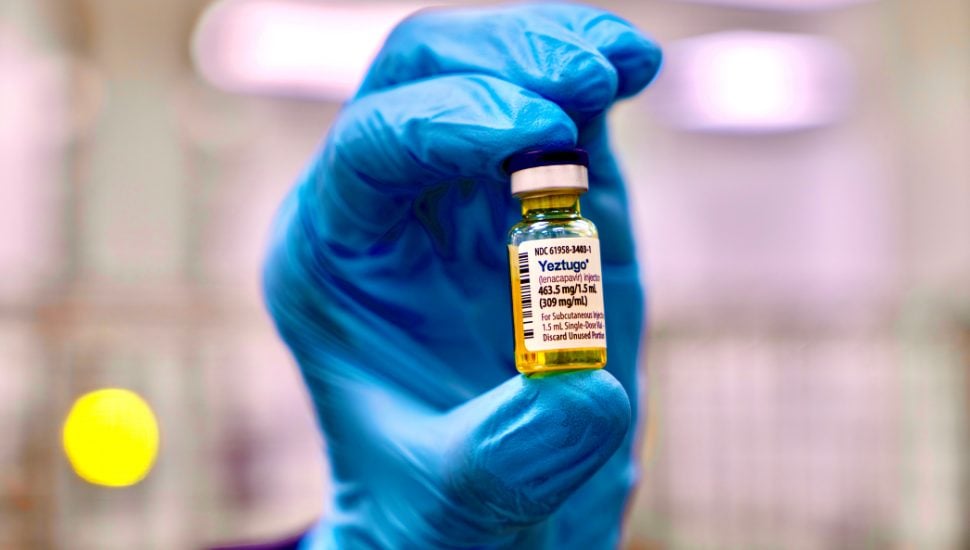
Some vaccines even prevent cancer, like the human papillomavirus (HPV) vaccine. HPV is one of the most common sexually transmitted infections, and while many cases resolve on their own, others lead to cervical, anal, penile, and throat cancers. The vaccine works best before sexual activity begins, but adults up to age 45 may still benefit.
That same principle applies to hepatitis B. Each year, DAP Health marks World Hepatitis Day on July 28 with a community forum, highlighting two viruses that have shaped global health for more than a century: hepatitis B and hepatitis C. Hepatitis B, preventable with a vaccine since 1982, still affects 250 million people worldwide and is the leading cause of liver cancer. Hepatitis C, discovered about 30 years ago, has infected about 200 million people globally — but unlike hepatitis B, it’s curable. These events bring together community members, health workers, and advocates to raise awareness, share resources, and promote prevention.
Trusted local messenger
The rise in vaccine hesitancy isn’t driven by any evidence showing danger. If anything, the safety record for vaccines has grown even stronger. But misinformation spreads faster than facts, and social media platforms often reward provocative claims over proven science.
“It’s difficult to rebuild trust in vaccines, especially when it’s rooted in political identity or misinformation,” Kerkar says. “We have to continue to serve as a trusted local messenger.”
That makes it all the more important for health care providers, community leaders, and informed citizens to keep telling the truth: vaccination is a simple but impactful act of public health solidarity. Each shot protects not only the person who receives it, but also newborns too young for vaccines, cancer patients with suppressed immune systems, and elderly neighbors at higher risk for complications.
“At a time when it’s easy to feel powerless against global health threats, vaccines remain a clear, proven way to take action,” says Kerkar. “Anti-vaccine sentiment may have clouded the conversation, but the facts haven’t changed. Vaccines work. They save lives.”
If you’re not sure which vaccines you’ve had or when, you can find your records online. In California, click here to quickly check your vaccination history and make sure you’re up to date.
To make an appointment for you or a child to get one or more vaccines, please reach out to your DAP Health primary care provider or to their pediatrician.
If you and your loved ones are not yet DAP Health patients, and and are interested in joining the DAP Health family, click here.